Schizophrenia is a serious mental illness that falls in the general category of psychotic disorders. Psychotic disorders involve a loss of contact with reality, leading to abnormalities in sensation (e.g., hearing voices or sounds that are not there, seeing things that are not real) and in thought (e.g., believing ideas that are clearly false). Schizophrenia is the most common type of psychotic disorder. Because the symptoms of schizophrenia impact core human functions of sensation and thought, it is considered to be one of the most debilitating mental illnesses.
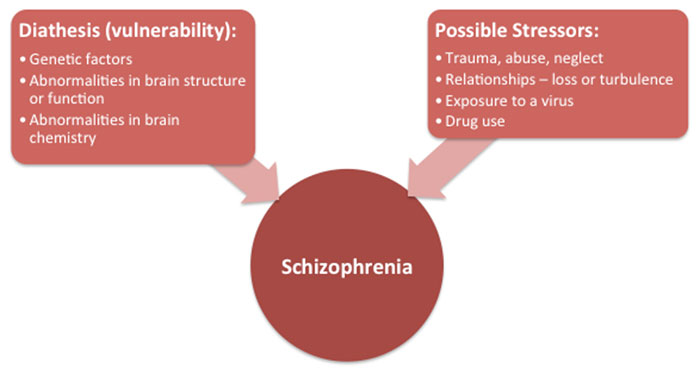
While scientific research has not yet found a clear-cut answer to what causes schizophrenia, it has been consistently found that the brains of people with schizophrenia tend to be different from individuals without schizophrenia, including abnormalities in brain structure and brain chemistry. Research also supports that schizophrenia is caused by a combination of both genetic/biological factors and environmental factors. This is depicted in the diathesis-stress model of schizophrenia below, which suggests that an individual with a biological vulnerability who then experiences a major life stressor is at the greatest risk of developing schizophrenia.
Schizophrenia is observed at approximately the same rate across cultures, with lifetime prevalence rates around 1%. Schizophrenia affects both men and women at approximately equal rates, though men typically begin to experience symptoms in their late teens or early twenties, while women tend to develop symptoms of the disease in their late twenties or early thirties.
Diagnosing Schizophrenia: Signs and Symptoms
There is no single laboratory measure or brain imaging test used for diagnosing schizophrenia. Rather, health care professionals use the criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM), which is currently in its 5th edition, for diagnostic purposes.
Diagnostic criteria for schizophrenia in the DSM-5:
A. Two or more of the following, with at least one being (1), (2), or (3):
- Delusions (beliefs that are firmly held despite strong evidence to the contrary);
- Hallucinations (a sensory experience of something that does not exist outside the mind, including seeing, hearing, feeling, smelling, or tasting something that is not actually there);
- Disorganized Speech (e.g., slipping off topic, going on a tangent, talking about things that seem unrelated or do not make sense);
- Grossly Disorganized or Catatonic Behaviour (e.g., displaying inappropriate emotional responses, having difficulty with daily activities such as self-care or cooking, not responding to the environment);
- Negative Symptoms (e.g., diminished emotional expression, decreased ability to start tasks, lowered motivation or drive, lack of interest in other people)
B. Disruption in Daily Functioning (e.g., difficulty at work, in relationships, or with self-care).
C. Continuous signs of the disorder for at least 6 months, with at least 1 month of the symptoms described above.
D. Other similar disorders have been ruled out, such as depressive disorder or bipolar disorder.
E. The disturbance is NOT related to drug use, medication use, or another medical condition.
F. If the person has a history of autism, they must also have prominent delusions or hallucinations to be considered to have schizophrenia.
Cognition in Schizophrenia
People living with schizophrenia often struggle with cognitive functioning, with most thinking skills typically being affected. For example, research has consistently shown that schizophrenia is associated with lower scores on tests of intelligence, and that this is generally apparent in childhood, long before the onset of the illness. Schizophrenia is also associated with difficulties in executive functioning (e.g., prioritizing tasks, planning, organizing, problem solving), memory, and thinking speed. Another cognitive symptom often associated with schizophrenia is lack of insight into the symptoms and/or severity of their illness. Additionally, research shows deficits in social cognitive abilities in schizophrenia (i.e., deficits in thinking about social phenomena). As a result, individuals with schizophrenia may have difficulty with things like comprehending and solving social problems or situations, labeling emotions, or understanding indirect speech such as sarcasm or irony.
Treatments for Schizophrenia
There is currently no cure for schizophrenia. The treatment plan should be tailored to each individual’s needs, given that the symptoms and course of illness vary on an individual basis. It is generally important to find the right medication to manage symptoms, with many different antipsychotic medications currently available on the market. However, the optimal treatment approach is generally one that combines both medication and psychosocial interventions, such as therapy or rehabilitation strategies involving work, school, and relationship goals. Family therapy may be used to improve family members’ knowledge of and coping with schizophrenia. Cognitive-behavioral therapy (CBT) may be helpful for some individuals, which includes developing coping strategies for dealing with symptoms and focusing on challenging firmly-held or negative beliefs. Notably, the majority of individuals with schizophrenia will experience repeated episodes of the illness throughout their life, even when receiving treatment. However, symptoms do tend to diminish with age, with the exception of cognitive deficits.